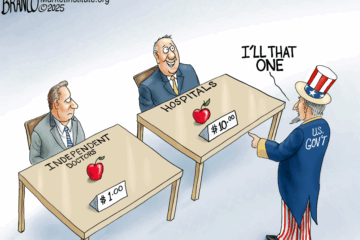
America’s largest government health programs are being quietly looted—not by patients, but by the very insurers trusted to manage their care. Through a practice known as upcoding, insurance companies inflate the severity of diagnoses to bill Medicare and Medicaid for more than what was actually needed. The result: billions in fraud, degraded care quality, and a growing hole in the federal budget.
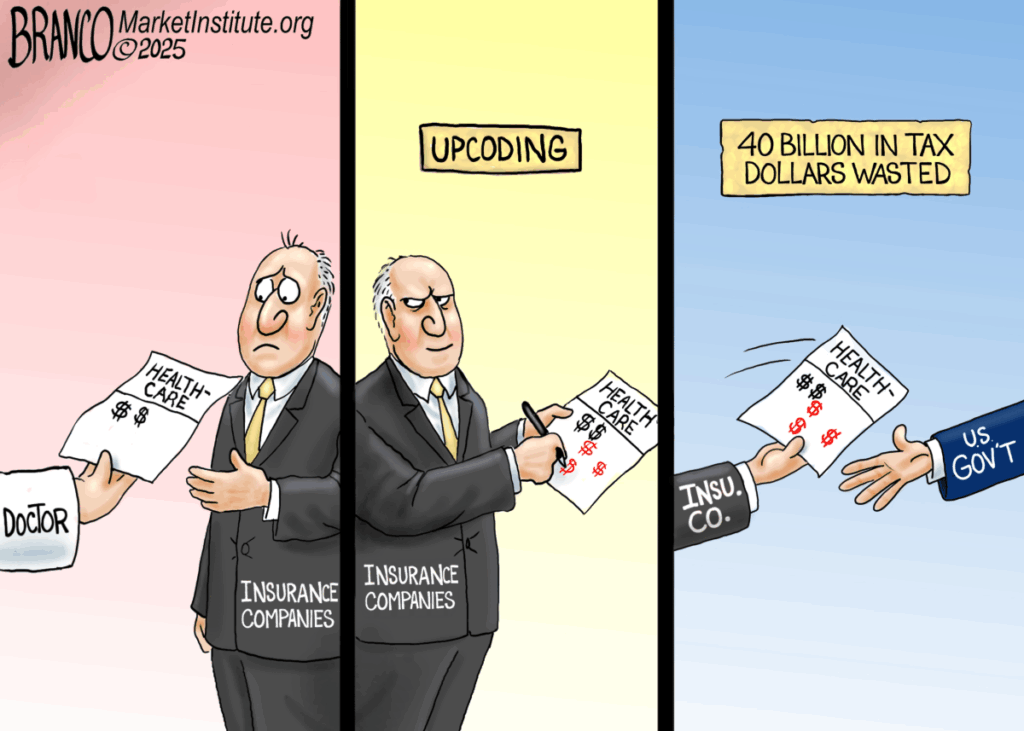
As detailed in our new report, improper payments are costing taxpayers up to $135 billion every year, driven by misaligned incentives, weak oversight, and systemic abuse.
Medicare Advantage alone saw $20 billion in overbilling in 2022, while Medicaid fraud topped $50 billion last year. And those numbers are likely low due to incomplete data from state agencies.
Until Congress fixes the incentives, fraud will keep winning and patients will keep paying the price.
MI-MA